
What Is Drug Resistance?
Drug resistance is the reduction in the effectiveness of a medication in treating a disease or condition.
When an organism is resistant to more than one drug, it is said to be multi-drug resistant.
Drug resistance is mainly noticed in Microbes known as antimicrobial resistance and in cancer known as Antineoplastic resistance.
The control of infectious diseases is seriously threatened by the steady increase in the number of microorganisms that are resistant to antimicrobial agents. Resistant infections lead to increased morbidity and prolonged hospital stays, prolonged periods of infections, and the spread of infections to other individuals.
Why Is It Increasing Globally?
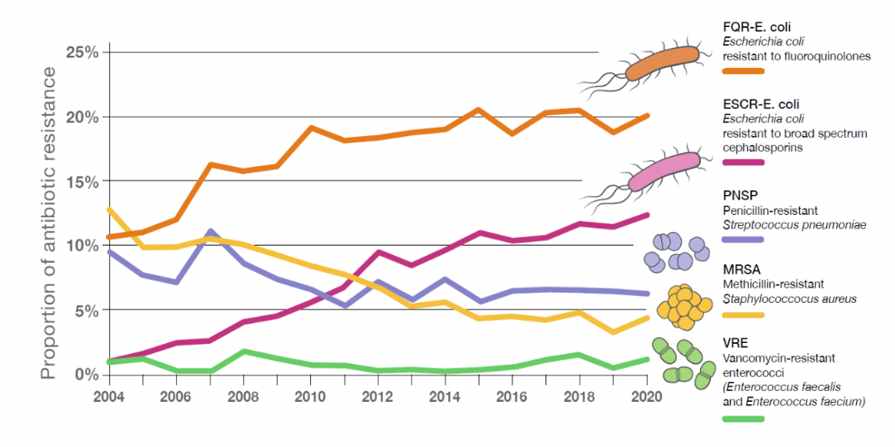
- Drug resistance infections have become increasingly prevalent nowadays. In developing countries, key contributors identified included Lack of surveillance of resistance development, poor quality of available antibiotics, clinical misuse, and ease of availability of antibiotics. In developed countries, poor hospital-level regulation and excessive antibiotic use in food-producing animals play a major role in leading to antibiotic resistance. India tops the list of countries with the highest antibiotic resistance. Already, drug-resistant diseases cause at least 700,000 deaths worldwide each year, but “if no action is taken,” that figure could increase to 10 million globally per year by 2050.
What Are The Mechanisms Of Anti-microbial Drug Resistance?
There are 2 types of drug resistance:-
- Internsic/natural resistance:
- Acquired resistance:
1. Intrinsic resistance: It is the intimate ability of a microorganism to resist a class of antimicrobials.
- Impermeability- For the antibiotics to affect the cellular process, they must penetrate the cell wall of the microbe. so, in drug resistance the cell wall becomes impermeable.
- Biofilms- Biofilms are sessile bacterial communities that are reversibly attached to a solid surface and embedded in an exopolysaccharide matrix. So, these biofilms decrease the penetration of the antibiotic.
- Efflux pump- These are naturally present in resistant microbes. There is an increased expression of the porin pumps due to the mutations, this leads to a greater exit portal for numerous antimicrobial agents.
- Enzymatic inactivation- Bacteria produce enzymes that destroy the antimicrobial agents before they reach the target.
2. Acquired resistance: The naturally suspectable microorganisms aquifers ways of not being affected by drugs.
- Efflux- Changes in the cell wall proteins can also result in novel acquired trait. In addition, some efflux pumps have translocated to plasmids, which can be acquired by horizontal gene exchange.
- Target site modifications- Modification of target sites can reduce the binding affinity of the antibiotic to the target.
- Acquisition of new target- Microbes also adapt to become resistant by acquiring the new cellular targets with reduced affinity for the antimicrobials.
- Enzymatic inactivation and destruction- The microbes acquire the enzymes that inactivate the antibiotics.
- Adaptation of alternative metabolic pathway- Antimicrobial These microbes adapt to another metabolic pathway so that the agent doesn’t work.
Which Diseases/Organisms Are More Prone To Drug Resistance?
The leading drug resistance diseases include:
- Mycobacterium tuberculosis
- Clostridium difficile
- Vancomycin-resistant Enterococci
- Methicillin-resistant Staphylococcus aureus
- Neisseria gonohheora
- Carbapenem-resistant Enterobacteriaceae
- Cancer
Mycobacterium tuberculosis- In the case of the TB regimen, it includes high doses of Rifampin, Isoniazid, Pyrazinamide, and Ethambutol for 6 months and resistance to these drugs is called multi-dug resistance tuberculosis. MDRTB is much more difficult to treat requiring expensive second-line drugs for at least eighteen months the optimal dose of levofloxacin is 750 mg once daily and that of moxifloxacin is 400 mg once daily.
Clostridium difficile- C. difficile is a pathogen infecting the colon of patients. CDI is typically caused by the exposure of the normal intestinal microbiota to antibiotics that are not active against C. difficile, which disrupts this flora and allows for the proliferation of C. difficile. Many antibiotics are associated with CDI; ampicillin, amoxicillin, cephalosporins, clindamycin, and fluoroquinolones continue to be associated with the highest risk for CDI.
Vancomycin-resistant Enterococci- Enterococci are commonly found in colonizing the human digestive tract and female genital tract. VRE infections tend to occur in people who are in hospitals or other health care facilities or susceptible to infection due to other medical problems or the presence of certain catheters or other devices. Health care providers commonly use the antibiotic vancomycin to treat Enterococcal infections, but VRE is resistant to the drug.
Methicillin-resistant Staphylococcus aureus- MRSA is one of the most common hospital-acquired infections. Increasingly, however, strains are circulating in the community and can cause severe infections.
Neisseria gonorrhoea- The bacterium that causes gonorrhoea is sexually transmitted. It can cause severe reproductive complications if left untreated, and it disproportionately affects sexual, racial, and ethnic minorities. Because some drugs like ceftriaxone and azithromycin are becoming less effective in treating gonorrhoea, the CDC recently updated its treatment guidelines to slow the emergence of drug resistance.
Carbapenem-resistant Enterobacteriaceae- CRE is a family of highly resistant bacteria that includes Klebsiella species and Escherichia coli (E. coli). CRE primarily affect patients in hospitals and those who have compromised immune systems. The bacteria can enter the body through medical devices like ventilators or catheters. Some CRE infections are resistant to most available antibiotics and can be life-threatening.
Cancer- Cancer cells will become resistant to drugs by the mechanisms such as the inactivation of the drug, multi-drug resistance, cell death inhibition (apoptosis suppression), altering in the drug metabolism, epigenetic changes, changes in the drug targets, enhances DNA repair and target gene amplification.
What Are The Causes Of Antimicrobial Resistance?


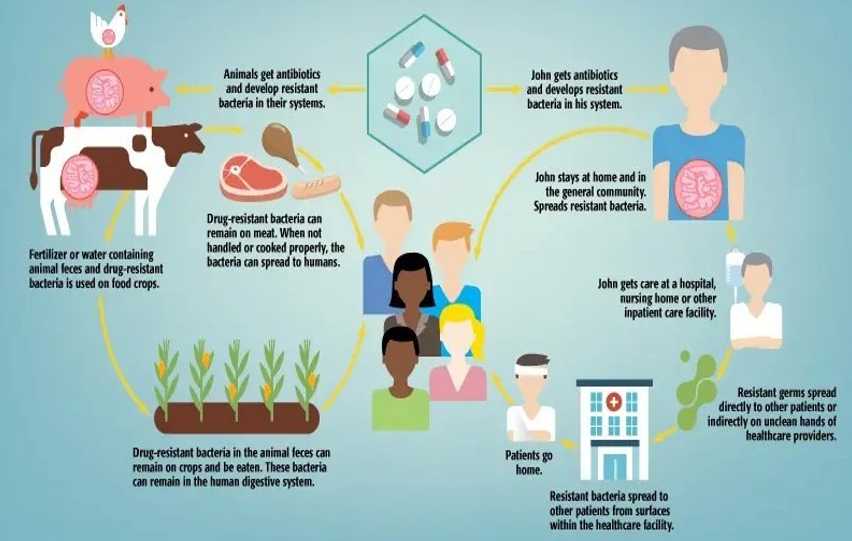
How Is Drug Resistance Transmitted?
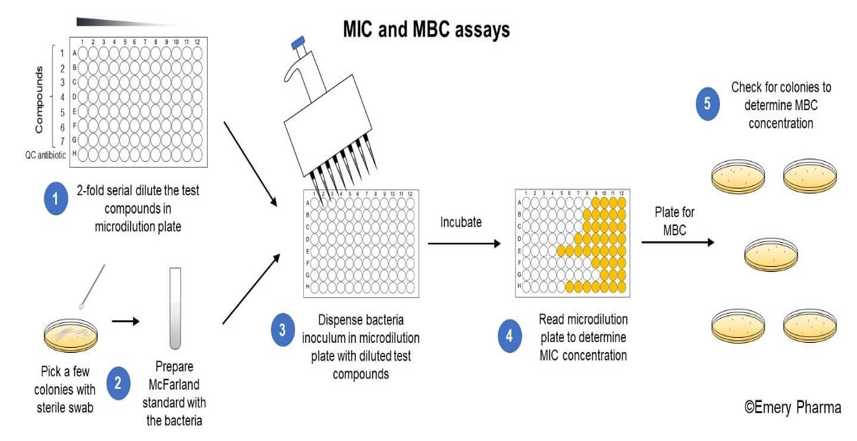
How Can We Diagnose Drug Resistance?
It can be done through 2 methods:
- Phenotypic method
- Genotypic method
1. Phenotypic Method:-
- This test estimates the phenotypic expression of resistance to one or more antimicrobial drugs. They include:
1. Agar Screen
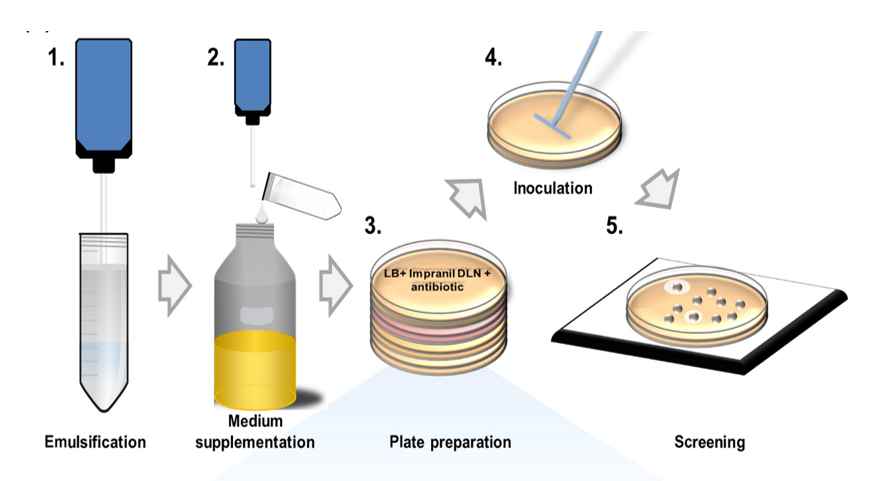
2. Disc Diffusion

3. MIC and MBC Assay
4. Automated Antimicrobial Susceptibility Test

2. Genotypic Method:-
- This test detects the genes or nucleotide sequences responsible for coding antimicrobial resistance. They include:
1. DNA Hybridisation

2. PCR Technique

3. Microarray Technique

What Are The Treatment Options For Drug Resistance?
1. Mycobacterium tuberculosis:
- Levofloxacin and moxifloxacin are the two most frequently recommended agents and the WHO has recommended the use of these drugs for the treatment of MDR-TB. The optimal dose of levofloxacin is 750 mg once daily and that of moxifloxacin is 400 mg once daily.
2. Clostridium difficile:
Antibody-based therapy.
A therapy, known as bezlotoxumab (Zinplava), is a human antibody against the C. difficile toxin B and has been shown to reduce the risk of recurrent C. difficile infection in those at a high risk of recurrence
3. Vancomycin-resistant Enterococci:
- Current treatment options including linezolid, daptomycin, quinupristin/dalfopristin, and tigecycline have shown favorable activity against various vancomycin-resistant Enterococcus infections.
4. Methicillin-resistant Staphylococcus aureus:
- Treatment of MRSA at home usually includes a 7- to 10-day course of an antibiotic such as trimethoprim-sulfamethoxazole, clindamycin, minocycline, linezolid, or doxycycline.
5. Neisseria gonohheora:
- Following the spread of gonococcal fluoroquinolone resistance, cephalosporin antibiotics have been the foundation of recommended treatment for gonorrhoea.
6. Carbapenem-resistant Enterobacteriaceae:
- Currently, antibiotic options for the treatment of carbapenem-resistant Enterobacteriaceae (CRE) are very limited, with polymyxins, tigecycline, Fosfomycin, and aminoglycosides as the mainstays of therapy.
7. Cancer:
- Combination therapy regimens are commonly used to overcome chemotherapy resistance in clinical trials. Overcoming Anticancer Drug Resistance—From the Drug Perspective. Simultaneous modulation of additional biological targets, or synergistic/additive activity against the same target, can be beneficial for treating malignancies that develop resistance to a particular group of drugs.
How Can We Prevent The Drug Resistance?

Top 13 Facts About Increasing Drug Resistance
Increasing Antibiotic resistance has been found in all regions of the world while India tops the list of countries with the highest antibiotic resistance.
Many people think antimicrobial resistance means antibiotics resistance; but Antimicrobials include antibiotics, antifungal, antiviral, and antiparasitic.
Resistance to even one antimicrobial drug can mean serious problems.
The greatest risk for antibiotic-resistant infections is young children, cancer patients, and people over the age of 60.
The more antibiotics are used to treat trivial conditions, the more likely they are to become ineffective for treating more serious conditions.
75% of Indians think incorrectly that cold and flu can be treated with antibiotics and 50% or more antibiotic prescriptions are inappropriate in several countries.
By 2050, 1 person could die every 3 seconds if Anti-Microbial Resistance is not tackled.
Nowadays antibiotics are given to food processing plants and animals; and in the case of animals, the drug-resistant bacteria get developed in their gut and reaches human through food, air, water, soil, or by direct human-animal contact.
Seventy years ago, before we had antibiotics, a simple cut or wound could kill because of a bacterial infection. Antibiotics changed that.
Almost 80% of patients hospitalized with COVID-19 received an antibiotic.
The first case of antimicrobial drug resistance was caused by penicillin and was observed in 1947.
Antimicrobial resistance leads to higher medical costs, prolonged hospital stays, and increased mortality.
Misuse and overuse of antimicrobials are the main drivers in the development of drug-resistant pathogens.
FAQs
Yes, antibiotic overuse is one of the leading causes of antibiotic resistance.
Yes, it’s one of the biggest problems. Increasing Antibiotic resistance has been found in all regions of the world while India tops the list of countries with highest antibiotic resistance. Antimicrobial resistance leads to higher medical costs, prolonged hospital stays, and increased mortality
Mycobacterium tuberculosis, Clostridium difficile, Vancomycin-resistant Enterococci, Methicillin-resistant Staphylococcus aureus, Neisseria gonohheora, Carbapenem-resistant Enterobacteriaceae are the organisms are more prone to drug resistance.
Yes, the drug resistance may be reversible. But it is very difficult to reverse the drug resistance.
Drug resistance can be developed by Internsic/natural resistance or Acquired resistance. Intrinsic resistance can be developed through the mechanisms like Impermability, Biofilms, Efflux pump, Enzymatic inactivation and Acquired resistance can be developed through the mechanisms like Efflux, Target site modifications, Acquisition of new target, Enzymatic inactivation and destruction, Adaptation of alternative metabolic pathway.
Yes, your body could be naturally immune to drugs and it’s known as drug tolerance. Drug tolerance occurs when someone’s body no longer responds to a drug in the same way it once did. It happens when someone has been taking a certain drug for an extended period of time.






